
Psychological and Inflammatory Responses in Relapsed/Refractory Patients with Chronic Lymphocytic Leukemia (CLL)
This research examines psychological (e.g., stress, depression), physical (e.g., fatigue, pain, sleep disturbance), and inflammatory (e.g., IL-6, TNF-alpha, vascular endothelial growth hormone, etc.) variables and their covariation in patients with relapsed refractory chronic lymphocytic leukemia (CLL) receiving a novel drug therapy, Ibrutinib.
Leukemias are cancers of the blood, bone marrow, and lymphatic system. Acute leukemias are characterized by rapid onset, progression, and probable death if left untreated. Chronic leukemias, on the other hand, are often characterized by a slow, insidious onset but some patients can survive many years.
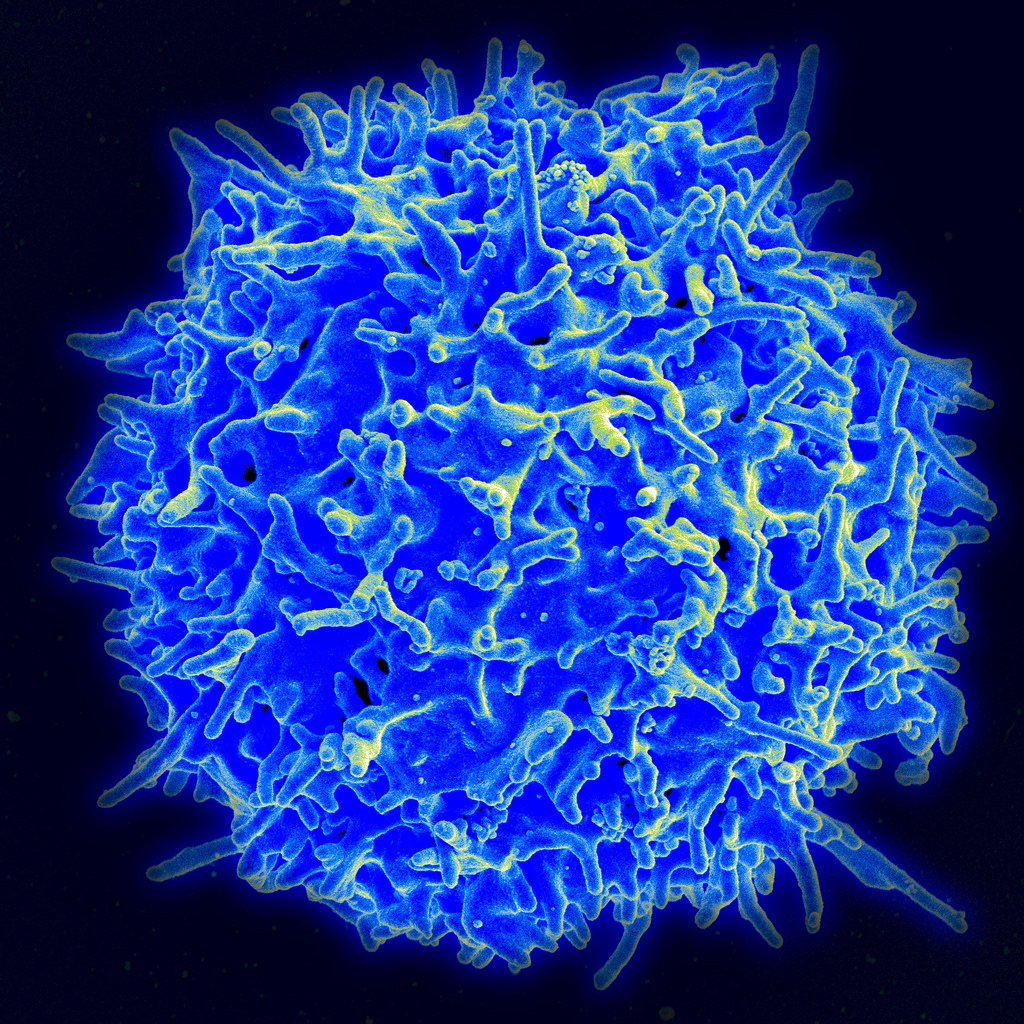
Many individuals with chronic lymphocytic leukemia (CLL) will have indolent disease for a substantial period of time, but the majority of patients will eventually require treatment. Currently, CLL is incurable. Front line treatments are effective and usually stave off disease progression, but all patients eventually relapse and become refractory to treatment. As patients pursue additional treatment options, the available therapies become increasingly toxic and less efficacious. However, Ibrutinib is a new, promising treatment. It is an orally administered inhibitor of Bruton's tyrosine kinase, an essential enzyme involved in the proliferation of abnormal lymphocytes. Ibrutinib has been shown to induce durable responses with minimal toxicity, and has recently been approved by the FDA. In collaboration with hematology oncology and basic scientist researchers, we study changes and interactions of psychological and physical outcomes and inflammation during the course of Ibrutinib therapy. To our knowledge, this is the first biobehavioral study of patients with CLL.
The From Cancer to Health™ Biobehavioral Intervention Training for Mental Health Care Professionals
As noted in the 2008 Institute of Medicine report, Cancer care for the whole patient: Meeting psychosocial health needs, the psychological distress of the vast majority of cancer patients is not addressed, posing a serious problem for the U.S. health care system. The NCI has acknowledged this by designating supportive care and quality of life issues of cancer survivors as health priority areas. However, progress has been limited by the poor availability of empirically supported treatments (ESTs) that can produce psychosocial and health benefits for patients. Unfortunately, there are few mechanisms for supportive care professionals to receive training in evidence based psychological treatments.
To address both gaps, NIH funding has provided for the From Cancer to Health™ (C2H) training program for mental health professionals. Funding has provided for 8 (2011-2016) three-day C2H training institutes for competitively selected (N=320) psychologists, social workers, and mental health clinical nurse specialists. The curriculum is the empirically supported Biobehavioral Intervention (BBI), offering training in stress reduction, communication with health care providers, social support, problem solving, health behaviors, sexuality, and maintenance of change.
Research shows the treatment to produce robust and positive, enduring gains for cancer patients. A randomized clinical trial of BBI with newly diagnosed regional (stage II or III) breast cancer patients (N=227), demonstrated significant reductions in patients’ emotional distress, improvements in social support, treatment adherence (chemotherapy), health behaviors (diet, smoking), and symptom and functional status, enhanced T cell immunity, and reduced risk for cancer recurrence.
The Institutes are the basis for ongoing research regarding the processes of dissemination and implementation of BBI. The Institutes are evaluated with a multi-level plan, with the first benchmarks being trainees’ knowledge gains in BBI and clinical expertise in delivery. Next, the extent of trainees’ clinical usage (implementation) of BBI is documented. Lastly, the research includes an open label (phase II) trial of the BBI as disseminated to and implemented by trainees on patient outcomes. The latter is collaborative research with selected trainees (C2H-Dissemination; see below). The overarching goal is to train supportive care professionals in the use of the BBI in order to improve care of cancer patients and survivors by the delivery of empirically supported treatment. Our early data suggest our effectiveness in doing so (Brothers et al., 2015).
From Cancer to Health™ Dissemination Project (C2H-D)
As described above, NIH Funding has provided for the From Cancer to Health™ (C2H) training institute for mental health providers to learn how to deliver the Biobehavioral Intervention. In addition to the training aim, a dissemination aim evaluates the effectiveness of the intervention as delivered by the newly trained providers on their patients’ outcomes. The From Cancer to Health™ Dissemination Project (C2H-D) is a multidisciplinary collaboration between the PI (Andersen) and former C2H trainees across the United States. Trainee/researchers currently come from Indiana University Ball Memorial Hospital, Baylor Research Institute, East Alabama Medical Center, Tahoe Forest Cancer Center, and others. Having successfully completed C2H training, they now provide BBI at their home institution. Moreover, they are research-collaborators, each collecting data from their own patients treated with BBI. For this, OSU serves as the Data Coordinating Center.
Thus far, no dissemination trials of empirically-supported psychological intervention for cancer patients have been conducted. If successful, the protocol will provided much-needed evidence on the effectiveness of the intervention on patient outcomes when delivered as disseminated to mental health professionals. Publications emanating from this program evaluation will be authored by the C2H-D Collaborative Group.
This page is maintained by the Arts and Sciences Technology Group. For technical help please email asctech@osu.edu
© 2015 Stress and Immunity Cancer Projects. All Rights Reserved. 159 Psychology Building 1835 Neil Avenue Columbus, OH 43210 P: 614.292.8429